"Behavioural dermatology - The Combined Approach to atopic eczema"
from exchange National Eczema Society Members' Magazine MARCH 2011 pp20-22
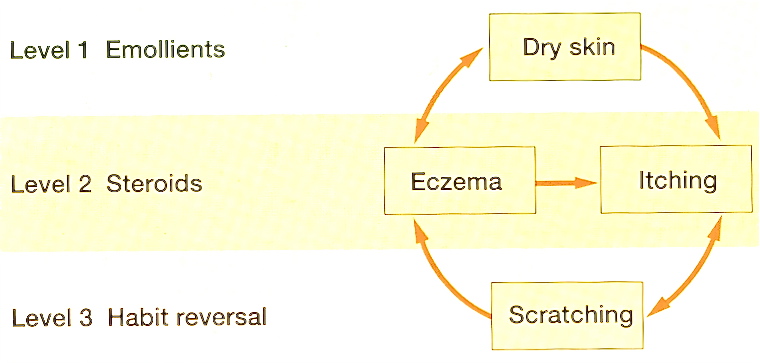
Behavioural medicine - of which behavioural dermatology is a part - links medicine with human behaviour, in order to both improve our understanding of physical illness, and therefore improve its treatment. Behavioural medicine takes account of the behaviour of everyone involved - those in need of care, and also those who provide care, both informally and formally. If behaviour is neglected the results of medical treatment can be less than satisfactory. When behaviour is accounted for, the results of treatment can be optimal.
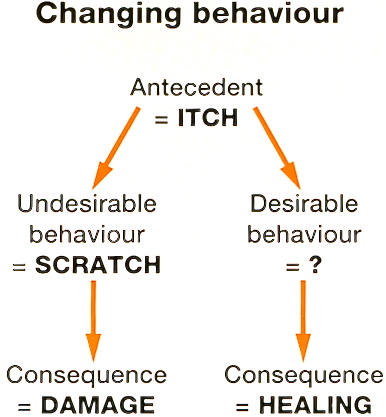
Behaviour therapy - a form of behaviour modification - is a treatment based on how we learn to do what we do, including how we feel and think, as well as act, in different circumstances. Behaviour therapy works by recognising how some habitual behaviour can be helpful, but also how some can be unhelpful and counterproductive - maladaptive: then, how improved results can be achieved by successfully learning new adaptive behaviour. As therapy, the behavioural approach has much in common with education and training. It is an attractive approach because it is easy to understand. It works by focusing on doing and practicing what is agreed as positive and helpful, rather than dwelling on what is negative and unhelpful. A new way of doing something in a particular context replaces an old way, making the old way impossible to carry out. This produces a desired effect which then reinforces the new behaviour: learning occurs.
 |
Although the combined approach is suitable for all ages, most of the people we have seen at Chelsea & Westminster Hospital have been either adults or teenagers. All have had atopic eczema for a long time and have been at least moderately affected, including major effects on quality of life and psychological well-being. We believe it is important that this demoralising state of affairs is recognised and taken account of at initial assessment. Active participation in a treatment regime requires a positive attitude, and a commitment to becoming an confident expert at using what is a self-help technique. We have been delighted by our results. It is important and relevant therefore that, right from the start, we share our enthusiasm for the approach with all who come to us for treatment.
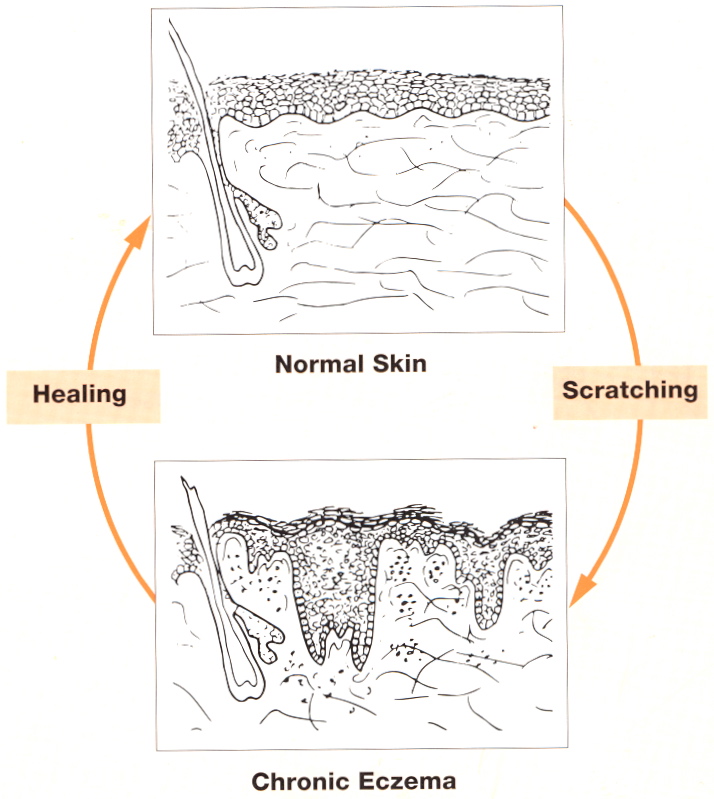 |
A key initial question is asked: "What percentage of your scratching is due to itch?". In a series of 50 consecutive patients before treatment we found a mean 60% of scratching was attributed to itch: the rest is caused by a variety of issues and factors, including stress, opportunity, boredom, frustration and tiredness - but not itch! Habitual behaviour begins with a specific conscious response to a particular stimulus - at first, the scratching is due to itch. As time passes however and the behaviour continues, it becomes relatively automatic and unconscious, and generalizes from being a specific response to itch to being a general response to a wide range of factors which varies from person to person. Such scratching or self-grooming is normal and instinctive - and often goes unnoticed: it is unconscious. It cannot however be taken for granted, if chronic atopic eczema is going to be successfully treated.
 |
 |
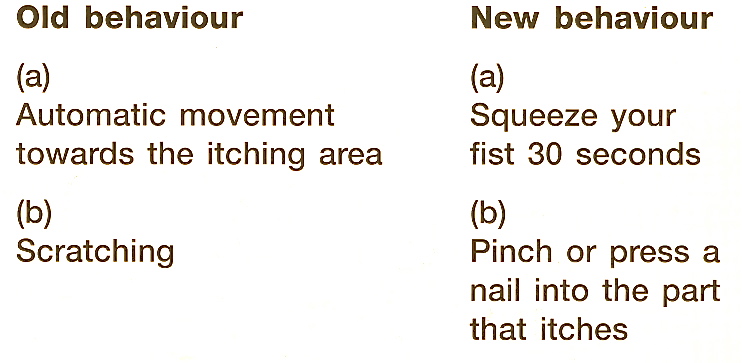 |
General measures to aid habit reversal take account of particular circumstances. Thus, planning ahead, doing things quickly, and keeping ones hands busy are all important. Each person has their own behaviour to modify, developing habit reversal principles to suit their own needs.
After another two weeks, the fourth clinic visit provides an opportunity to review the programme, and to make individual adjustments. Usually emollients can now be continued as needed, topical steroids are discontinued at the correct point, and with scratching frequency now less than 10 episodes a day, habit reversal and the use of the tally counter are no longer required. Now it is important to understand how future episodes of acute eczema can be provoked, how they can be recognized, and how they need treating early and vigorously with increased emollient use, and a short course of topical steroids - without habit reversal. This will clear acute eczema in three or four days, the chronic eczema having needed as many weeks - with habit reversal. As the next three months pass, episodes of acute eczema become less severe and less frequent, as the skin recovers further. Our patients now report feeling positive and confident, both regarding the management of their eczema, and regarding life in general.
Outcome study
A follow up audit of 37 patients who followed the combined approach programme enabled us to review outcome after one year, in 26 patients - 76% showed greater than 75% improvement in skin condition, while 81% reported greater than 75% improvement in their quality of life. Achieving treatment goals, with continuing only intermittent use of topical steroids as detailed above, was reported by 70%.
Conclusion
The combined approach to the management of chronic atopic eczema can be successfully offered by nurses and doctors, both in dermatology clinics and in general practice settings. It is also feasible for some as a self-help treatment programme. Sue Armstrong-Brown, one of our patients at Chelsea and Westminster, has written such an account: it contains much more detail of the treatment programme, for those who are interested to know more.
Reference
- The Combined Approach to atopic eczema is attractive because it is easy to understand.
- It is an exercise in guided self-help, involving learning how to optimise conventional treatment and how to eliminate habitual scratching using habit reversal.
- As a treatment programme it involves a series of steps taken over several weeks, with positive results within one month.
